How the Pandemic Changed HR’s Views on Virtual Care
This year we’ve heard a lot about the sea change regarding virtual medical care. From a predicted increase at the beginning of the pandemic, we saw...
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
.png)
The US healthcare system is overwhelming for the average employee. When choosing the wrong primary care provider can mean thousands in out-of-network penalties, how are individuals meant to handle the bigger decisions, like managing a chronic illness?
The truth is, Americans are ill-equipped. One study found that 60% of US adults have low health literacy. The study also noted that there are disparities among age groups, genders, ethnicities and income levels. The bottom line is – people don't have the right information or tools to navigate today's healthcare system.
That means worse health outcomes over the short and long term. It also means higher costs for individuals and the companies sponsoring their health benefits. Companies spend 30% of total headcount expenses on benefit programs.
Employer healthcare costs are climbing. In 2024, the cost to insure an individual employee topped $8,400, and just under $24,000 for a family. While employers pass some of the premium to the employee, they ofter shoulder most of the burden themselves.
At the same time, enrollment in high-deductible health plans is steadily increasing year over year, raising the stakes for employee finances.
Increasing healthcare costs put your employees at risk. For 2025, out-of-pocket maximums for families may reach as high as $16,600, yet the average American doesn't have $400 in savings. Low health literacy is associated with increased, repeated emergency room visits and unfortunately, worse health outcomes, according to the University of Florida College of Medicine.
And these increases in cost are an existential threat to businesses, as well. Since employees simply don't have the right knowledge or tools, they don’t feel responsible for how their healthcare choices impact their employer’s bottom line.
Employers who want to finally control their skyrocketing healthcare costs don’t need a one-off cost-containment measure or a new wellness program. Point solutions won’t solve the problem, and education alone isn’t enough to prompt employees to make smarter healthcare choices. To truly drive behavioral change, employers need an always-on, approachable tool that helps their people identify, access, and interface with the right healthcare every step of the way.
They need a better way to help their employees get care. This is where a healthcare navigation platform comes in.
A healthcare navigation platform connects people with the right providers, services, and support at the right moment in their healthcare journey to positively impact both their health and the cost of care.
Employees who don’t understand their benefits are likely to turn to costly options for care. For instance, they may choose a hospital imaging facility over a lower-cost standalone facility, simply because it’s in the same hospital network as the prescribing provider.
With a healthcare navigation solution, employees benefit from tools that make it easy to find the right care, including on-demand support, care redirection, and steerage to lower-cost virtual care solutions. HealthJoy clients achieve significant hard-dollar savings thanks to these features within the HealthJoy smart care navigation platform.
A healthcare navigation solution can prompt employees to remember preventive screenings and improve healthcare outcomes through early detection. Employees who don’t understand their benefits are avoiding or delaying care, and that leads to worsening health outcomes.
Encouraging employees to engage in preventive activities is about ease of use. Employees put off these activities for myriad reasons, including fear, forgetfulness, lack of time, and low understanding. A healthcare navigation solution breaks down these barriers. It not only reminds employees to take care of themselves, but shows them how to do so. The right connected care experience can seamlessly transition employees from a push notification to scheduling an appointment without ever moving to another app or website. With tools like 24/7 access to live healthcare concierge support and case management, they never have to walk through their healthcare journey alone.
A healthcare navigation solution isn’t just about finding savings on big-ticket items, like surgery or imaging. It can also prompt engagement with your preventive measures, like wellness programs, fitness challenges, virtual primary care, and more. These programs head off higher costs, but are often limited by low utilization.
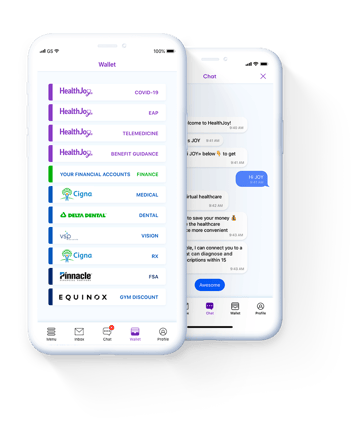
When you implement a fully-connected navigation platform that’s integrated with your benefits package, you’ll gain access to tools that make your wellness benefits more approachable. Everything is easily displayed when they open the app, and timely push notifications can draw attention to your health and wellness initiatives more effectively than email. A mobile care navigation platform also unlocks personalized communication tools HR can use to send out timely reminders and announcements, whether related to new wellness initiatives or open enrollment.
With higher participation and engagement, your wellness programs can yield more ROI and greater employee satisfaction. In other words, a healthcare navigation platform can actually make all your benefits more valuable.
When every piece is working together to make health and wellness easier, a healthcare navigation solution’s effectiveness should speak for itself. With the right solution, companies will notice a decrease in healthcare spending, as well as improved satisfaction and benefits engagement from employees.
Employees don’t know how to find cost-effective care, which drives up both their out-of-pocket costs and your company’s expenses. Point solutions can address problems from different angles, but without a connected experience, they fall flat.
Here’s why.
Healthcare decisions are stressful. Asking employees to make smart, informed choices at the time of a stressful healthcare event isn’t reasonable. Employees need support for every healthcare decision, throughout the year, without hours of research.
Point solutions don’t work together, meaning employees must access a different site, download a different app, or call a different number for every resource. This siloed experience only increases confusion and frustration. As more point solutions flood the benefits landscape, there’s still a need for solutions that bring them together.
A fragmented benefits experience makes it harder for HR to meet their goals. Juggling a maze of vendors is difficult for employees and your team. Each vendor requires a different implementation experience, provides a different level of support, and means a different navigation experience for employees.
A healthcare navigation solution solves these problems. With a connected benefits experience, employees can intuitively find the right care at the right time. Live, personalized guidance and an approachable interface make a confusing system more human. And when employees can make smart healthcare decisions with ease, healthcare costs go down — for them, and for your company.
HealthJoy is a benefits and care navigation platform that makes healthcare easier for your employees to access, navigate, and afford. Our engagement engine and dedicated team of healthcare concierges unite to guide members to get the best care at the best price—so your benefits work as designed.
Want to learn more?
DISCLAIMER: This blog was originally published in 2022 and was updated in 2025.
This year we’ve heard a lot about the sea change regarding virtual medical care. From a predicted increase at the beginning of the pandemic, we saw...
When an employee takes family leave, there are many things HR needs to do along the way. There are legal guidelines you need to follow under the ...
The COVID-19 pandemic irrevocably changed the world of work. For employers, it meant re-evaluating existing business models and placing a renewed...