Introducing HealthJoy’s Virtual MSK Care
Chronic pain can be a pain. For an estimated 126.6 million Americans suffering from a musculoskeletal (MSK) condition, finding a better way to...
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
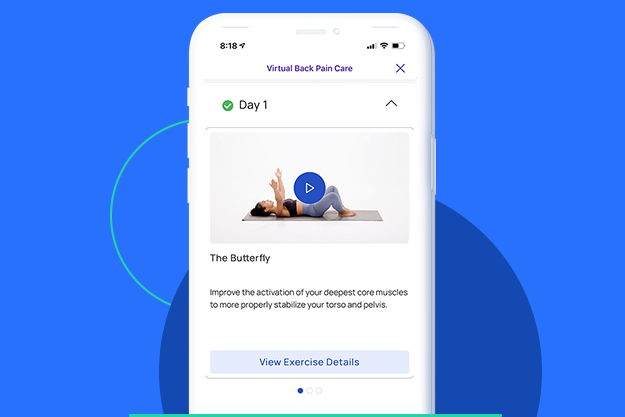
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy

Today I’m pleased to tell you a little more about HealthJoy TPA+, an innovative new solution for Third Party Administrators (TPA’s) to leverage insights and AI and simplify their members’ path to care.
You might already know that HealthJoy’s benefits experience platform integrates with a client’s existing benefits package to deliver each employee a personalized, proactive experience. Employees gain access to on-demand medical consultations, live healthcare concierges, Rx savings, and much more.
Our new TPA+ product expands this core offering by bringing claims, insurance verification, and precertification data into the mix. Using this data, our AI-powered virtual assistant, JOY, proactively engages our TPA+ partners’ members with guidance to high-quality, fair-priced care. In short, TPA+ helps us offer timely personalization and navigation assistance to our members at scale.
During my time at HealthJoy, I’ve consistently seen TPA’s miss the opportunity to put their remarkable wealth of data to good use. We all know healthcare costs are climbing, yet we can’t jump in to change consumer behavior.
For instance, a TPA might grant precertification to a doctor for a knee replacement surgery. They know that a few key choices in the scheduling process could mean a difference of thousands of dollars in employer costs and employee cost-sharing. Yet they have little to no way to offer guidance to the employee before they decide where to seek care.
Instead, the TPA is forced to watch while an employee chooses a facility and a provider. Without the proper tools on their side, member engagement is impossible.
That’s where HealthJoy TPA+ comes in. It allows HealthJoy to deeply embed in our TPA partners’ member experience. We’ll see insurance verification and precertification data on a daily basis. That gives JOY and our concierge team time to proactively assist members, reaching out to reinforce a great choice or suggest a higher-quality and/or lower-cost care option.
With HealthJoy TPA+ employers have a new level of access to member decision making, which means they can get very strategic with cost-containment strategies. On the backend, through a monthly claims integration, employers also receive reporting showing how member engagement with the plan strategy is resulting in savings. How about that? Better member experience and better healthcare transparency!
The marriage of our technology and our partners’ data is key to creating a more meaningful benefits experience. Digital transformation occurs because they make experiences simpler, more affordable, and more personalized. This product accomplishes all three of these for our members and self-funded employers. We expect the outcome of HealthJoy TPA+ partnerships will be revolutionary for our industry.
HealthJoy TPA+ is launching with an exclusive list of partners this summer, including Auxiant, Coastal Administrative Services, and Loomis. New partnerships will be available in the fall.

Chronic pain can be a pain. For an estimated 126.6 million Americans suffering from a musculoskeletal (MSK) condition, finding a better way to...

At HealthJoy, we believe that privacy is your fundamental right. We design every technical system, process, service from the ground up to...

2024 is set to be our most ambitious year to date in the HealthJoy product organization. With so much going on, I wanted to be sure to provide you...