How HealthJoy Gets in Front of Healthcare Decisions
For an employee, navigating the healthcare system is just a series of difficult decisions. With unclear pricing and confusing deductibles, it’s...
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy

With so much conversation surrounding the broken U.S. healthcare system, we often overlook what this brokenness means for patients themselves. Our patchwork system of insurance carriers, TPAs, employers, brokers, and private doctors and facilities translates into a messy patient experience. Healthcare’s different players don’t communicate or collaborate over a single unified platform, which means patients must struggle to connect the dots between their insurance coverage, choices of doctors, and employee benefits. The result is a healthcare experience that is overwhelming, disunified, and much more complicated than it needs to be.
Today’s patient experience is like watching a dysfunctional baseball team play. The players don’t communicate, they are unable to share key information with one another, and each player has different motivations. We, as the audience members, must bear one loss after another and unhappily sit through a game that we can only describe as a poor viewing experience. Breaking apart and investigating each symptom of the broken healthcare experience is the best way to develop an effective treatment.
The key to any winning team is a strong flow of communication between its members. Expectations should be clear, and collaboration must be convenient for the team to achieve outstanding results. Unfortunately, players within the healthcare system utterly lack the ability to communicate with each other.
Siloed communication is one of healthcare’s worst inefficiencies. Doctors, insurance companies, and employers have no easy way to interact on a consistent basis. This means your doctor doesn’t know your insurance plan, prescription formulary, or whether they’re referring you to an in or out-of-network specialist. They’re unsure of a drug’s formulary tier or what the pharmacy you are going to will charge, so sometimes you’re in for a shock when it comes time to pick up a prescription. The average doctor visit is only 15.7 minutes long, so don’t expect them to be able to figure it out either.
When doctors and hospitals don’t communicate with payers (employers, TPAs, and insurance carriers), it’s almost a guarantee that the healthcare experience will be inefficient and overpriced. The communication dilemma can be solved simply by providing a space where healthcare players can congregate, much like a team dugout where teammates gather. From achieving faster treatment approval from insurers to eliminating wasteful duplicate testing, a mode of communication between healthcare players would drastically improve the patient experience. No one is at the center of the typical healthcare experience and helps the member.
While weak communication is one issue, a lack of data-sharing between healthcare players is a whole other beast. There’s no shortage of data in healthcare: doctors, insurers, hospitals, and third-party administrators all have huge repositories of data. What is lacking is the flow of data between these players. Instead of having free-flowing information across the various systems involved in care, we are stuck with information silos that make it hard to leverage the data in a useful way. On a macro level, patient data can allow researchers to identify important indicators like health trends and patient care best practices.
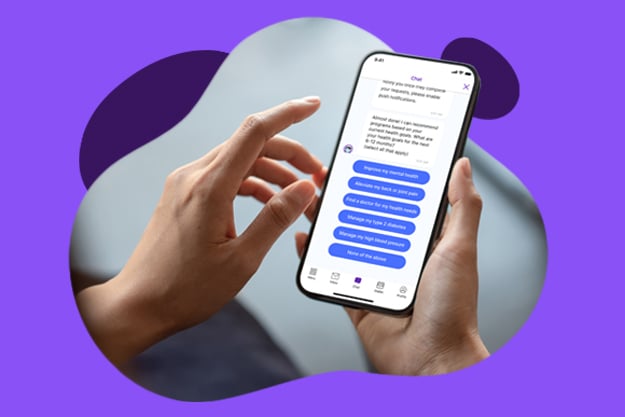
From the level of individual patients, a lack of integrated data systems makes it hard to be a consumer of healthcare services. When visiting the doctor’s office, patients don’t remember basic information like whether they have reached their deductible, what their past claims have looked like, and how much their insurance will cover for a given treatment. If this is the case, how can we expect them to be able to choose appropriate care? Patients need access to their health data wherever they are and whenever they need it to make fully-informed decisions. This information also needs to be presented in an easy to understand manner, but even if this happens patients either need a lot of education or on-demand guidance.
When put to good use, the possibilities for data to improve the patient experience are endless. Data that is properly harnessed can drastically lower healthcare costs, from recommendations on prescriptions to rerouting care to less expensive facilities. Opportunities for care based on industry best practices after analysis of data is an occasion to help patients become not only healthier but lower costs.
Right now, most patients enjoy little to no personalized or digital access to their data. Instead, they receive cryptic postal mailings or access to web portals that are more troublesome than helpful. The difficulties of finding and accessing one’s data are one of the worst parts of a patient’s experience and may lead people to feel as though the system is working against them. While industries like online shopping, social media, and entertainment are all racing to provide consumers with highly personalized experiences, healthcare services are not evolving nearly fast enough. While the digitization of our lifestyles is becoming the norm, many traditional institutions within healthcare push back on this inevitable change. This leads us to the 3rd symptom of our broken patient experience– conflicts of interest.
The traditional model of healthcare, which is usually described as “fee-for-service,” motivates providers to treat the largest number of patients in the shortest amount of time. Naturally, this approach leads to overtreatment, substandard quality of care, and overall low patient satisfaction. Thankfully, the old payment model of “more is better” is slowly being replaced by value-based models of care, such as accountable care organizations, which give providers monetary incentives to provide quality over quantity.
While incentives are being shifted for the better, many players in healthcare are still holding on to the traditional system because they fear what innovation will mean for them. Doctors may want to provide high-quality care, but fear what will happen if demand for their services goes down. To be lifted by the shifting tides of digitization, doctors must also embrace popular telemedicine opportunities that enable them to see more patients without the wasteful amount of paperwork and appointment scheduling. Insurers and third-party administrators may fear the consequences of their data becoming more transparent, but they should keep in mind all the ways that analytics and artificial intelligence can make their jobs easier and give them more time to focus on critical tasks. Ultimately, fixing the patient experience doesn’t mean patients win, and others lose. Rather, a more efficient system that harnesses modern technology will result in a better experience for all players.
After diagnosing the patient experience, we can see that it is in a critical condition. The individual today is a ping pong ball in an ecosystem of different incentives and siloed datasets of the broker, employer, carrier, and the provider.
It’s time we redesign healthcare experience to cater to the patient’s experience, rather than to the insurers who hold the purse strings, or doctors who possess the medical expertise. Just as every successful company puts the customer experience first, healthcare must also adopt a patient-centered approach. After all, the entire reason the industry exists is to improve the patient’s health and well-being. The best part about improving the system, however, is that everyone who’s part of the system will benefit. We are embarking on the “Age of the Patient,” and healthcare players must decide on whether they will adapt or go the way of the dinosaur.
For an employee, navigating the healthcare system is just a series of difficult decisions. With unclear pricing and confusing deductibles, it’s...

If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
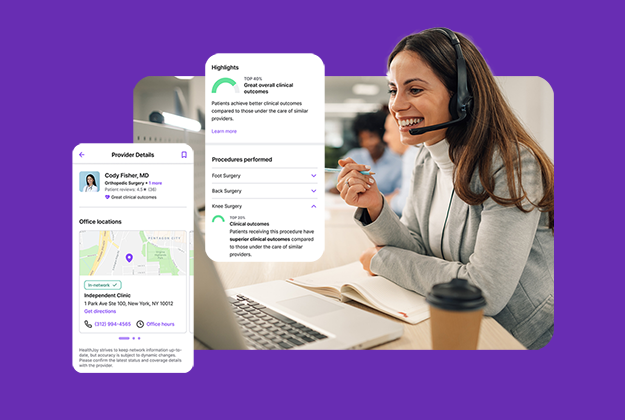
A crucial part of a high-quality benefits experience is ensuring that employees can access the high-quality care they need, without breaking the bank...