Why is benefits engagement crucial for healthcare cost containment?
If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
3 min read
Kevin Hyland
:
April 9, 2024
With health insurance costs continuing to rise—and the largest increase in health insurance costs in a decade expected this year—employers are exploring all possible options to contain costs.
With the search for savings more important than ever, we’ve seen a boom in point solution adoption. Point solutions provide a convenient way—via an app or digital tool—for organizations to fill gaps in the benefits they offer. Because of the rapid growth in this space, thousands of new employee benefit point solutions have emerged in the past several years.
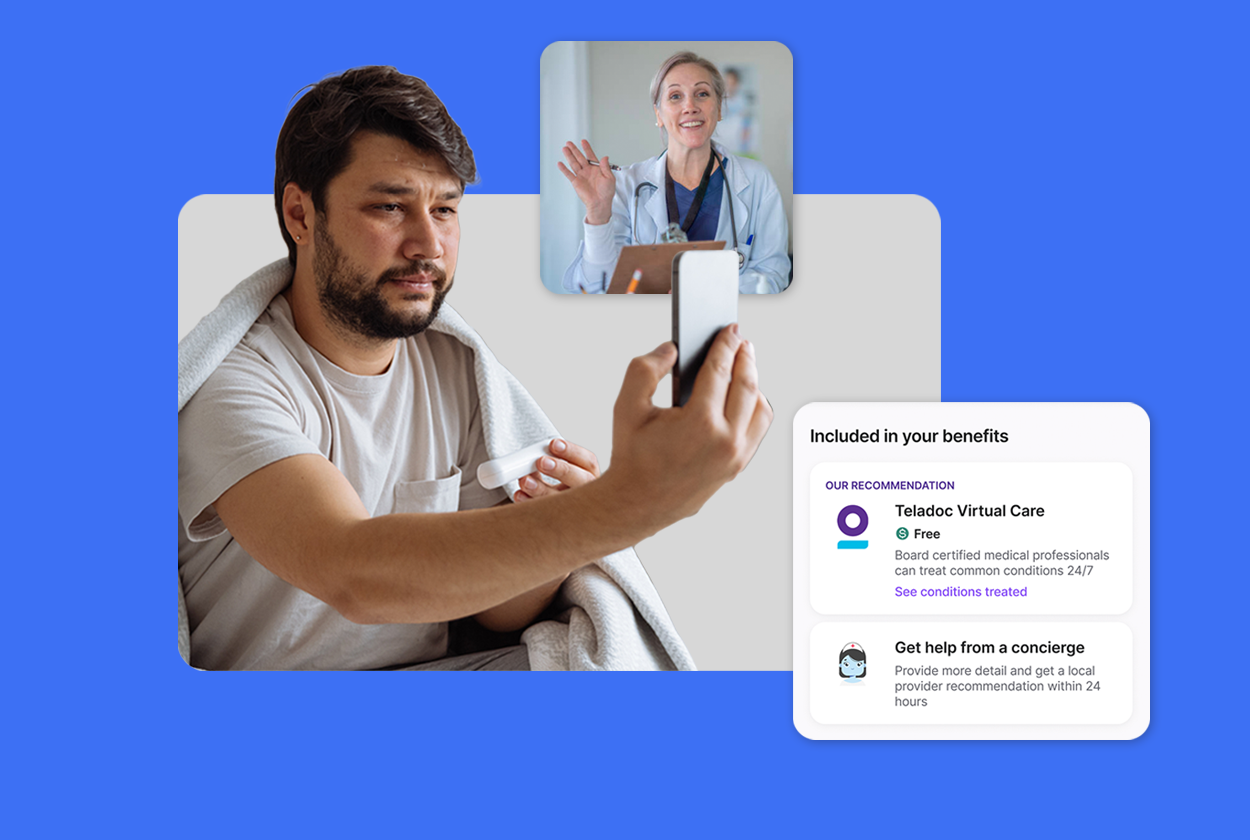
Many of these point solutions offer virtual care to employees. According to the Kaiser Family Foundation, 96% of employers now offer telemedicine solutions as a benefit. The American Medical Association confirms this rise on the provider side as well, noting that 74.4% of physicians surveyed reported that Telehealth was used in their medical practices—nearly three times the rate in 2018.
Just how prevalent have virtual care and point solutions become? Nearly 50% of organizations currently offer between four and nine separate point solutions.
The broadening of benefits programs comes with pros and cons.
Greater access: New, innovative solutions often provide employees with greater access to care.
The ability to offer more robust benefits offering, which increases benefits satisfaction
These solutions help accelerate cost containment when appropriately utilized.
Employee confusion: They may be confused about where to turn when they need care. This leads to low utilization (and understanding) of benefits and poor member experience.
Employees may be experiencing point solution fatigue and abandon their benefits altogether due to the overwhelming amount of options.
Complex and confusing benefits programs can be difficult to manage and administer.
These programs don’t integrate, creating a fragmented and confusing employee experience.
Few opportunities for personalization within the employee benefits experience.
Simply put, the success of a benefits strategy relies on employee benefit utilization. When employees don’t understand the benefits available to them—or the value that they could potentially provide—they’re much less likely to use them.
When employees don’t use the benefits provided to them the ROI of these programs dwindles and the strategy falls short. Employee utilization is crucial in impacting cost savings for employers and their employees.
By boosting employee utilization, HealthJoy drives 21% lower spend for high-cost claimants
Savings and improved health outcomes aren’t the only benefits of high utilization. High utilization rates indicate that employees are engaged and value the benefits being offered by their employer.
This can lead to increased levels of employee satisfaction and help employers with employee retention.
HealthJoy uses a combination of smart navigation technology and human-guided support to drive activation, ongoing engagement and, ultimately, better health outcomes for employees.
Here's a look at how HealthJoy drives utilization from activation through onboarding and beyond.
Activation: Our approach to supercharging engagement starts before a member even activates the app. HeathJoy executes member marketing email campaigns and provides educational resources to be used during open enrollment, pre- and post-launch as well as throughout the year to drive activation.
Onboarding: When a member activates HealthJoy, we capture their health goals and existing health needs to personalize the benefits experience through our Member Health Goals questionnaire.
Ongoing Engagement: Using a combination of personalized in-app health recommendations, concierge support, clinical coach outreach and push notifications, we keep employees actively engaged in their health. We help employees locate in-network medical, dental and vision providers to best fit their needs. But to make sure we’re surfacing the most cost-effective option, we look across the entire benefits package pulling in virtual care options when available.
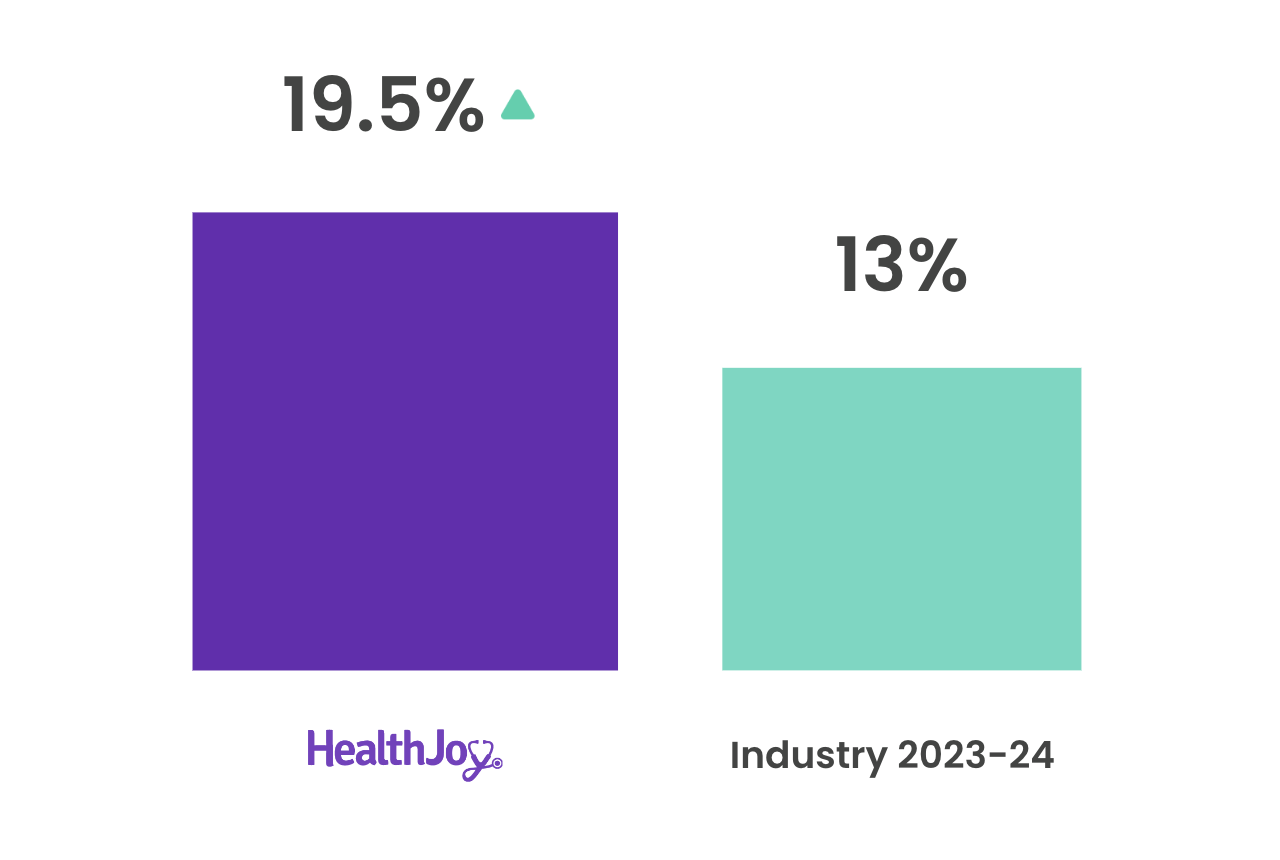
HealthJoy transforms healthcare outcomes by amplifying benefit strategies and streamlining the employee experience. By doing so, we’re actively removing the complexity and confusion that has historically overwhelmed employees. The result? 50% higher utilization rates than our industry benchmark.
This annualized utilization rate (19.5%) was calculated based on HealthJoy's clients who had used Teladoc's General Medical solution for 12+ months.
Calculating this involved multiplying the total number of consults within the specified timeframe by the ratio of the total accrued months to 12. Then, the resulting figure was divided by the total number of eligible primaries. Finally, the calculated rate was compared to the industry utilization benchmark of 13% for similar-sized mid-market TPAs.
When utilization rates rise by 50%, savings and satisfaction usually follows for both employers and employees.
As healthcare costs continue to rise, HealthJoy is committed to guiding employees to affordable, high-quality care options while helping employers contain costs.
Learn more about how HealthJoy can help bring your benefits strategy to life.

If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
%20(1).png)
Another renewal season is on the horizon and for many, this one feels different. HR leaders and the benefits consultants they work with are feeling...

The second annual Member Health Goals report harnesses the power of data to help discover the differences between the type of benefits employees...