Why is benefits engagement crucial for healthcare cost containment?
If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
3 min read
 Melanie Powell
:
April 10, 2024
Melanie Powell
:
April 10, 2024
A crucial part of a high-quality benefits experience is ensuring that employees can access the high-quality care they need, without breaking the bank (for themselves or their employers). But when employees don’t have the knowledge or proper tools to find highly-rated, in-network providers – along with cost comparisons – it’s difficult to make informed decisions about their healthcare.
The benefits experience can be confusing for employees. To address rising costs, benefits programs are becoming broader. “On average, large employers and plan sponsors have nine or more point solutions as part of health and wellness benefits.”
There are pros and cons to this marketplace (point solution) boom. While these solutions can lead to cost containment when appropriately utilized, having all of these programs can create a fragmented experience — causing confusion for employees.
At HealthJoy, we set out to address the complexity by bundling an unbundled benefits experience and eliminating the confusion that comes with it.
Another important piece of the experience is ensuring employees receive the best care, at the most affordable price.
In 2024, employers are bracing for the largest increase in healthcare costs in a decade, with estimates as high as 8.5%. To prepare for this increase, many employers have rolled out various cost containment strategies. However, the problem is, many of these initiatives prove to be ineffective.
While these strategies are rolled out with the best intentions, it’s not uncommon for them to add a layer of complexity to already confusing benefits programs. When employees feel confused about what benefits are available to them or how to access them, it leads to low utilization, and a cost containment strategy is only effective if it’s being used.
Another issue with some cost containment strategies is that they are not personalized to employees’ unique wants and needs. Employees aren’t one size fits all, so their benefits experience shouldn’t be either. In fact, fewer than 20% of adults in the United States know the cost of their healthcare products or services before receiving them, and almost all of them believe health care organizations need to make costs more transparent.
In the following sections, we’ll tell you how we’re reducing healthcare spend for employers and employees through our recent enhancement to HealthJoy’s Find Care search tool.
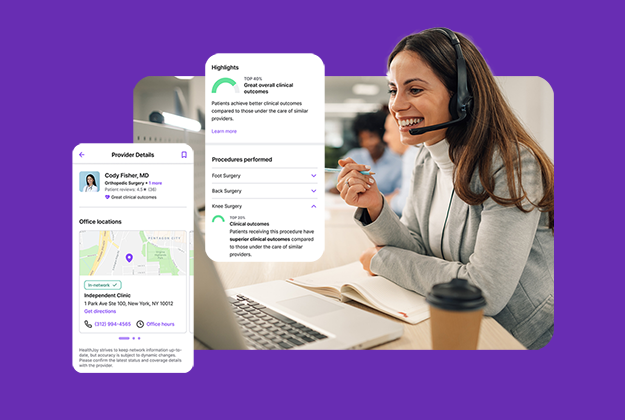
We help employees locate in-network providers and facilities across their medical, dental and vision plans – including other relevant benefit programs – in a matter of minutes.
Our Find Care search tool brings cost and quality information directly to employees through a seamless, self-service experience by:
We’ve partnered with Ribbon Health, a leading healthcare data platform, to incorporate cost and quality data into provider and facility searches. This data integration enhances the employee experience by providing upfront cost and quality data for providers and facilities across the entire benefits package – and specifically highlights upfront costs from the member’s healthcare network.
Our Find Care feature also reduces the number of touchpoints employees need to identify and reach the right provider and facility to meet their needs – simplifying the experience and saving them time.
Employees are less likely to delay care when they’re able to easily find high-quality, in-network providers when and where they need them. By seamlessly connecting employees to high-value care, we help employers mitigate catastrophic claims and reduce healthcare spend by 21% for high-cost claimants.
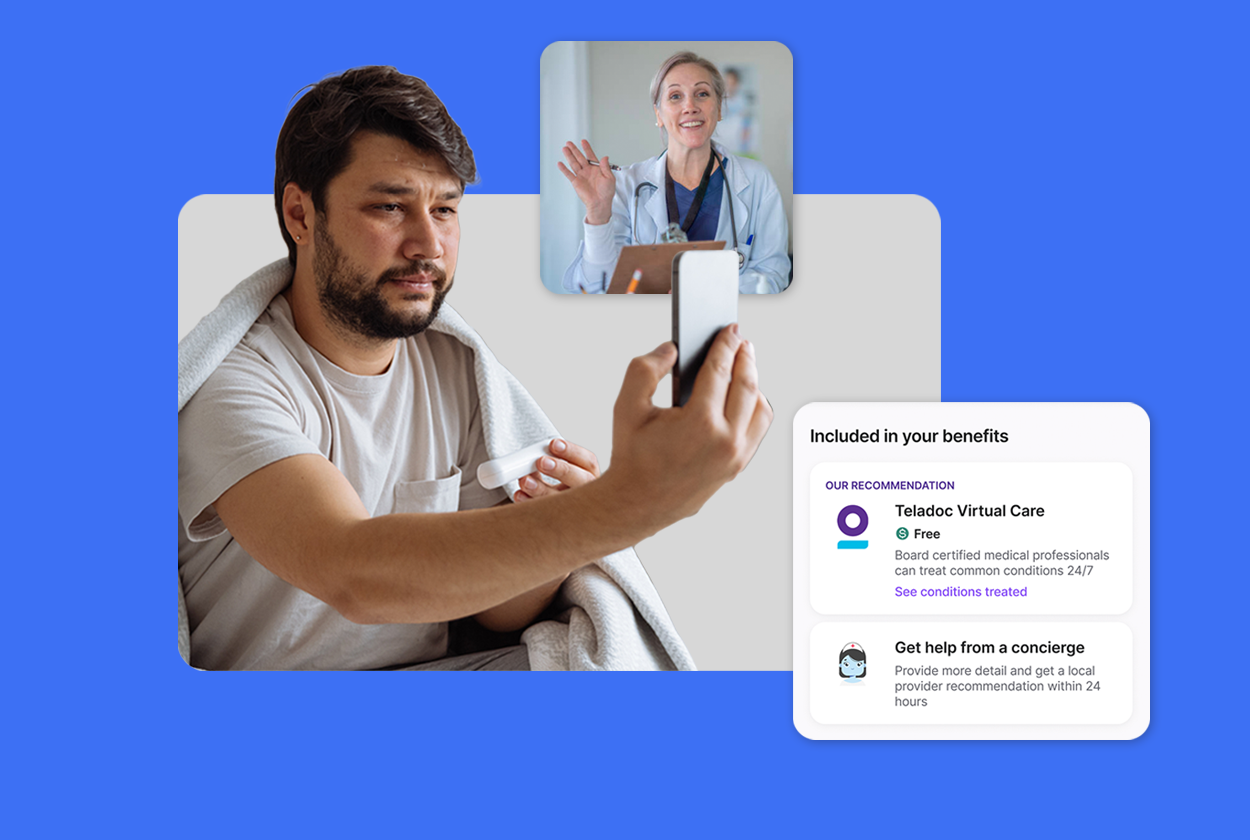
We put employee preferences at the center of our Find Care experience. Employees can use this comprehensive provider and facility search tool as a self-service option or connect directly with our healthcare concierge team for human-guided support.
Our healthcare concierges continue to provide support for members even after the initial appointment has occurred. They help employees by scheduling follow-up appointments, identifying prescription savings options and even reviewing medical bills before payment due dates.
The combination of a trustworthy, self-service provider and facility search experience, coupled with the personalized support from our healthcare concierges, improves the employee benefits experience and increases point solution utilization 2-3x.
Benefits engagement is an issue many employers struggle with. Employees often don’t know exactly what benefits are available to them, let alone where and how to access them. With HealthJoy’s Find Care search tool, employees are seamlessly guided to the optimal benefits and care to meet their needs – whether that’s finding a specialist, utilizing their dental or vision plans or accessing virtual care programs or onsite clinics.
This personalized steerage increases benefits engagement and helps employers achieve increased utilization rates. And by steering employees towards cost-saving care options like telemedicine, not only do employees end up spending less out of pocket, but employers can reduce their healthcare spend as well.
Sometimes, an unintended consequence of rolling out new benefits strategies is the administrative burden that is placed on the HR team. HR professionals have a lot on their plates already, and when employees misunderstand their benefits, they use the HR function as their go-to source for help.
HealthJoy relieves some of that administrative burden. Our solution is proven to save HR teams 142 hours annually per 100 employees. When the employee benefits experience becomes simplified, and employees are given both self-service options and dedicated support from our healthcare concierges, the burden on HR is reduced significantly.
A key part of HealthJoy’s mission has always been to guide employees to the highest-quality, most affordable healthcare. We work every day to help our members locate in-network providers and facilities across their health plan and other benefit programs.
Our enriched Find Care experience takes the guesswork out of healthcare decisions, by surfacing the most affordable care options – to optimize savings for the employer and employee, and by recommending the most highly-rated providers to improve health outcomes.

If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.

2024 is set to be our most ambitious year to date in the HealthJoy product organization. With so much going on, I wanted to be sure to provide you...
Benefit programs are becoming broader With health insurance costs continuing to rise—and the largest increase in health insurance costs in a decade...