Digital Solutions, Analog Delivery: The Hidden Failure Point in Healthcare
When I talk to CEOs, I always start with the same question: Do you know how much you are spending on healthcare? The universal answer is “Too Much”.
Connected Navigation Platform
Guiding to high-value care
Behavioral Health
Foster a mentally healthy workplace
EAP
Supporting holistic wellbeing
Virtual MSK Care
Reimagining musculoskeletal care
Virtual Primary Care
Powered by smart navigation
Surgery Centers of Excellence
Best-in-class surgical outcomes
Virtual Urgent Care
Immediate care, any hour of the day
Chronic Care
A new approach to chronic care
Integrations
Flexible to any strategy
3 min read
 Melissa McDonald
:
July 28, 2024
Melissa McDonald
:
July 28, 2024

If you are responsible for managing employee benefits – phrases like “healthcare costs are skyrocketing” are the soundtrack narrating your work day.
In 2024, employers are projected to pay an average of $18,000 per employee family - roughly the price of a Honda Civic.
Poor healthcare literacy isn’t helping matters.
Despite being well-versed in ordering DoorDash food delivery and using Uber to catch a ride from the airport, employees need help navigating the complexities of healthcare.
A 2022 Policygenius survey revealed that over one-third of respondents had avoided care or treatment because they didn’t understand their health insurance coverage.
When employees avoid or delay care, it increases healthcare costs for themselves and their employers.
To impact healthcare spend, employers must focus on benefits education and engagement.
A recent study by the International Foundation of Employee Benefit Plans (IFEBP) found that companies with high levels of employee engagement in benefits programs experienced healthcare costs 20% lower than those with low engagement.
To summarize: better benefits engagement = better utilization = cost savings.
In this post, we’ll explain how HealthJoy tackles long-term healthcare spend by keeping employees engaged in their benefits.
Benefit strategies are reliant on employee engagement and utilization to be successful.
Employees are much less likely to use benefit offerings when they don’t understand what’s available and the value.
When benefit offerings and cost containment solutions go underutilized, the return on investment falls flat – impacting the overall strategy.
When benefit offerings and cost containment solutions go underutilized, the return on investment falls flat – impacting the overall strategy.
HealthJoy brings benefit strategies to life – to improve health outcomes, contain healthcare costs and deliver a benefits experience that employees value.
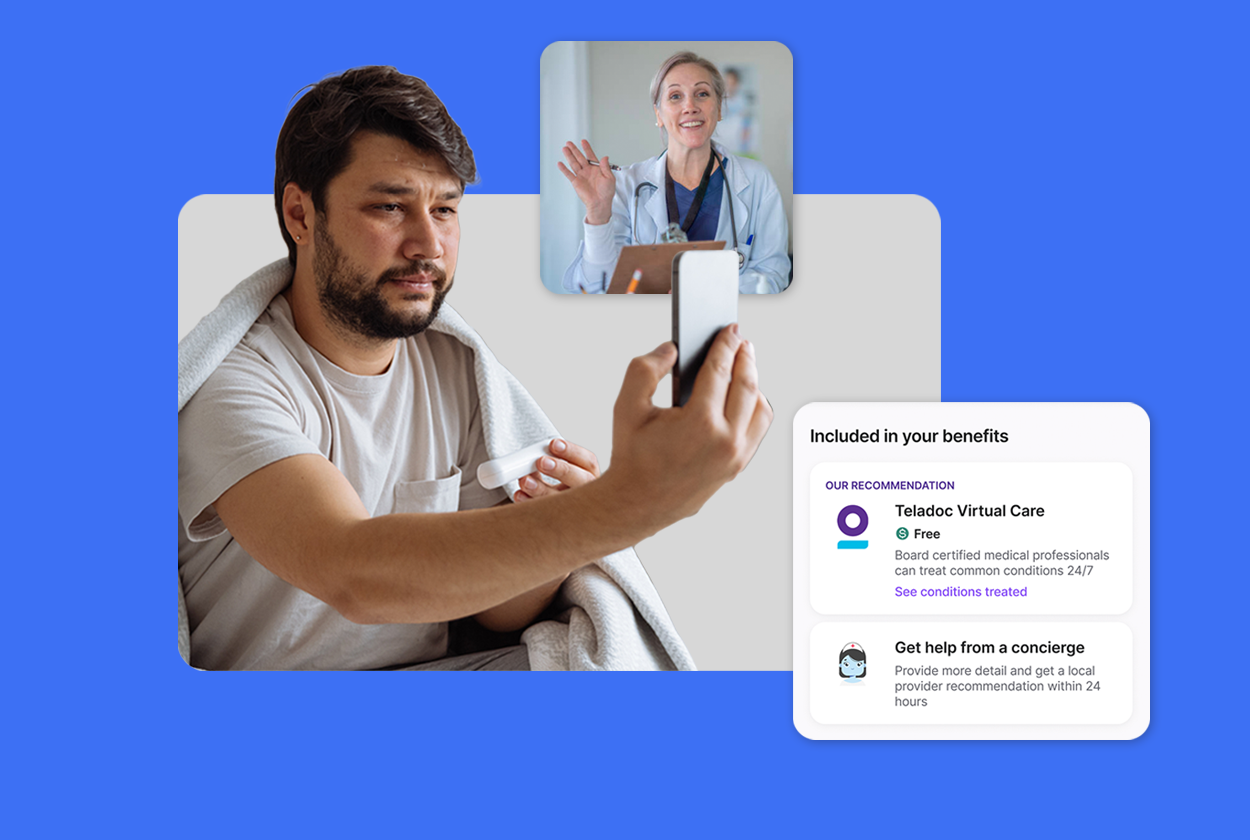
Our smart care navigation platform and human concierge team unite to make healthcare easier for employees to access, navigate and afford.
We start by bundling all benefit offerings – integrating all solutions regardless of vendor – to amplify an employer’s total rewards strategy. This gives employees one place to go for any healthcare question, challenge or need.
Then we map data to build an employee’s health profile to adapt the benefits experience to their wants and needs. Our virtual care integrations make it simple to connect employees to the best care across the entire benefits package and drive 50% higher telemedicine utilization than the industry average.
By steering employees to the highest-quality, most affordable care, we power an employer’s ability to confront long-term healthcare costs.
Here's a look at how HealthJoy drives utilization from activation through onboarding and beyond.
Activation: Our approach to supercharging engagement starts before a member even activates the app. HeathJoy executes member marketing email campaigns and provides educational resources to be used during open enrollment, pre-and post-launch as well as throughout the year to drive activation.
Onboarding: When a member activates HealthJoy, we capture their health goals and existing health needs to personalize the benefits experience through our Member Health Goals questionnaire. After employees submit their goals, they receive a personalized health plan tailored to their wants and needs.
Ongoing Engagement: Using a combination of personalized in-app health recommendations, concierge support, clinical coach outreach and push notifications, we keep employees actively engaged in their health and boost benefits utilization by 2-3x.
By driving better benefits engagement and higher utilization HealthJoy helps HR teams tackle their toughest benefits challenges and the associated costs.
Helping Employees Stay On-Track with Preventive Care
HealthJoy uses in-app reminders and push notifications to remind employees to get their annual physicals. Regular check-ups, screenings and vaccinations are essential for catching health issues early before they become costly to treat. By getting ahead of health issues, we reduce healthcare costs associated with expensive emergency room visits and chronic disease management.
Promoting In-Network Care Providers
HealthJoy brings provider cost and quality information directly to employees through a comprehensive, self-service search tool and our healthcare concierge team. Our Find Care experience takes the guesswork out of healthcare decisions, optimizing savings for employers and driving increased benefits utilization. Using in-network providers and facilities reduces the risk of unexpected medical bills, which can increase overall healthcare costs.
Driving Virtual Care and Third-Party Benefits Utilization
At HealthJoy, we’re passionate about connecting employees to high-value care. To do this, we help employees locate in-network medical, dental and vision providers to best fit their needs. But to make sure we’re surfacing the most cost-effective option, we look across the entire benefits package pulling in virtual care options and third-party benefit offerings when available.
Supporting Mental Health Needs
When an employee needs help, it should be easy to find. HealthJoy partners with Teladoc Health to provide high-quality virtual therapy services to adults and adolescents for a wide range of conditions. Layering HealthJoy's navigation solution onto Teladoc Health Mental Health maximizes enrollment and drives higher utilization.
Managing Chronic Conditions
Chronic conditions can be debilitating - physically, emotionally and financially. HealthJoy partners with Teladoc Health to help employers address the high prevalence of chronic conditions and associated costs. We centralize all chronic care programs into a single interface, offering a seamless member experience and in-app referrals to programs such as HealthJoy Rx Savings when needed.
Benefits engagement and utilization are proven to drive long-term healthcare cost containment. HealthJoy keeps employees engaged in their benefits by integrating all benefits, adapting to wants and needs and creating a premier care experience.
As healthcare costs continue to rise, HealthJoy is committed to guiding employees to affordable, high-quality care options while helping employers contain costs.
This post was adapted from content previously published in 2019 and 2024.

When I talk to CEOs, I always start with the same question: Do you know how much you are spending on healthcare? The universal answer is “Too Much”.

Employer healthcare costs climb every year. For individuals, the stakes are perhaps even higher.
Benefit programs are becoming broader With health insurance costs continuing to rise—and the largest increase in health insurance costs in a decade...